What is Insurance Verification in medical billing?
The health care industry provides medical care to thousands of people claiming to have health care insurance. It is because not everyone can afford the best treatments available in a hospital. However, many times people claiming to have health care insurance turn out to be frauds. Sometimes, they give wrong details about the insurance payer and avail medical care services at no cost. To prevent such false insurance claims hospitals make sure to get the insurance claim verified beforehand by outsourcing medical billing services. Medical billing is a service offered by medical billing companies to assist with various administrative tasks including verification.
So, what is insurance verification in medical billing?
Insurance verification refers to the process of verifying insurance claims to avoid fraud or denials. The process requires a professional to contact the insurance company/payer to verify the insurance claims. The procedure of verifying the insurance claims focuses on three major aspects—coverage status, active/inactive status and eligibility status. In addition to this Medical Insurance Verification Companies also help and keep tracking of account receivables. Not performing the verification thoroughly may result in the delay of payments.
The insurance verification service offered by medical billing companies is quite trustworthy. Outsourcing insurance verification allows the hospital to prevent their revenue cycle from getting affected. The team of experts provided by the medical billing company follows the following steps.
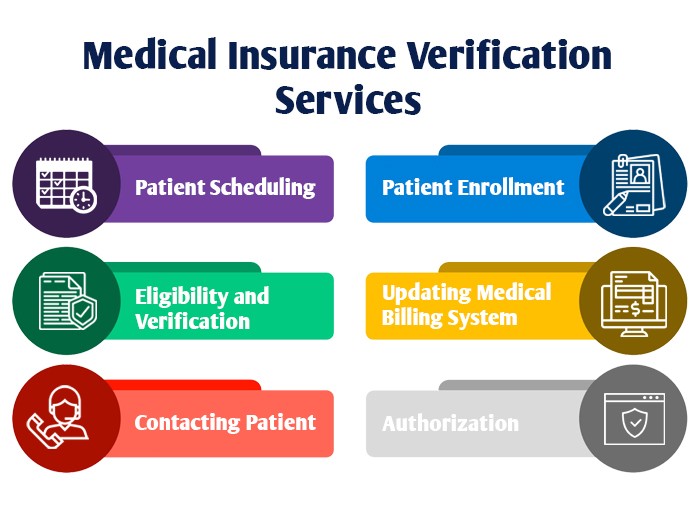
- Patient Scheduling– Registering the patient by gathering his/her details like appointment via texts, email or fax. It helps in marinating a systematic record, and no long queues.
- Patient Enrollment– It is important to gather the patient’s demographic details. This helps in identifying the patient and maintaining his/her medical history. It also helps the hospital to prevent insurance denials for the same information that can be used during insurance verification.
- Eligibility and Verification– The important procedure of cross-checking the detail of insurance claim is important to verify a patient’s eligibility for insurance.
- Authorization– It is essential to get the insurance company to authorize the insurance claim thus making it to pay the promised amount.
- Contacting Patient– It is important to update the patient about the status of the verification process.
- Updating Medical Billing System– The billing system is designed to keep a record of all the data associated with insurance verification.