What is a Clean Claim in Medical Billing?
Nothing is worse than glancing at your accounts receivable aging and seeing that services that were rendered months ago remain in the rejected/denied status.
In this case, you are a doctor, but since you are involved in a US healthcare business, you are also a business owner because your attention should be on patient outcomes. The single biggest bottleneck to a healthy cash flow is a misunderstanding of “what is a clean claim.”
Once a claim has been submitted to a payer, be it Medicare, Medicaid, or a private insurer, it has to be flawless so that it will be processed automatically. Otherwise, you do not get paid or even lose your money. In this guide, we will explain the medical definition of a clean claim and the reason why it is the lifeblood of your revenue cycle management (RCM). You will know how to avoid dirty claims and how to have a system that will enable your practice to remain profitable.
What Does a Clean Claim Mean in Medical Billing?
A clean claim in the context of medical claims and billing is simply a claim that a health insurance payer receives without any errors or omissions. However, let us take a closer look at the definition of a clean medical claim. According to the Health Insurance Portability and Accountability Act (HIPAA), a clean claim must contain all the required data elements necessary for the payer to process the claim under their specific payment system.
A claim is considered clean only when it can be handled by the automated system of the payer and no human being is required to pause, inspect the claim, and query, “What does this mean?” or “Where is the authorization number?” It must follow the standard 837 format for electronic submissions or the CMS-1500 form for paper.
To be considered a clean claim, it must meet these criteria:
- Complete Data: Every required field (patient name, DOB, insurance ID, NPI number) is filled.
- Accuracy: The ICD-10 diagnosis codes must match the CPT or HCPCS procedure codes.
- Timeliness: It must be submitted within the payer’s specific “timely filing” window.
- No Pending Attachments: It doesn’t require additional medical records or documentation for the initial adjudication.
Why are Clean Claims Important?
The significance of clean claims medical billing is critical. When your practice has a high first-pass yield (the percentage of claims paid on a first submission), then your cash flow is still predictable.
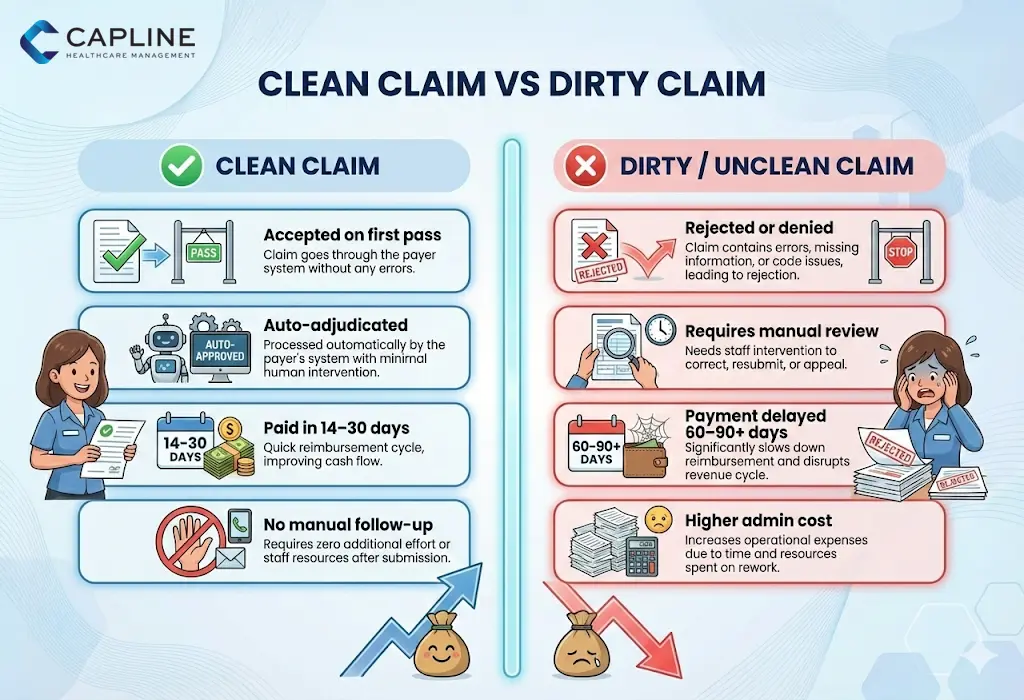
- Reduced Days in AR: You will receive payment in 14-30 days when you make a clean claim. This can be dragged to 60 or 90 days by unclean claims.
- Reduced Administrative Costs: Each time a biller has to lay their hands on a claim, you are compensating his/her time. Zero rework is needed when a clean claim is made.
- Better Payer Relationships: Clean data invariably lowers the chances of being warned of an audit.
What Causes a Claim to Be Not Clean for Billing?
A claim is said to be dirty or unclean when there is even a small mistake in it. Common issues include:
- Easy errors in the name or policy number of the patient.
- Lapsed insurance cover (lapse of non-eligibility).
- Missing or incorrect modifiers (e.g., forgetting a -25 modifier on an E/M code).
- Lack of a valid National Provider Identifier (NPI).
What Are The Steps Needed to Take to Ensure a Clean Claim?
The clean claim begins way before the biller hits send. It is an interdepartmental process that engages your front office, your clinical staff, and your billing team. Let’s begin
Step 1: Real-Time Eligibility Verification
The failure of the claim to pass the clean claim medical definition is most likely to happen because the insurance was not active during the date of service. You must verify at the time of scheduling and at the time of check-in.
Step 2: Accurate Documentation and Coding
Your providers must document the “medical necessity” clearly. In case a CPT code is submitted as a high-level visit, but the ICD-10 code does not cover the complexity, the claim is immediately dirty.
Step 3: Test Claim Scrubbing
Claim scrubbing in medical billing is your safety net. It is a software process that checks the claim with thousands of rules specific to payers before a claim is ever sent to the insurance company. It looks for:
- Gender-specific code conflicts.
- Age-specific code conflicts.
- Bundling issues (NCCI edits).
- Required attachments for specific procedures.
Step 4: Quality Assurance (QA) Review
Human intelligence and skills are usually necessary in high-value claims, even with the software. It is recommended to audit 5% of your claims each week at random to find systemic mistakes in your front-desk workflow.
How to Increase Your Clean Claim Ratio?
You are missing out on money if your present clean claim rate is less than 95. In order to improve on this, I would recommend:
- Invest in Staff Training: Have your front-desk members know how one slip of the typing on a group number can hold a $5,000 payment.
- Ensure Your Software is Updated: Your EMR/biller software is not up-to-date with the 2024-2025 ICD-10 code sets; you are putting yourself on the path to failure.
- Use Automated Scrubber Tools: Don’t rely on manual checks for medical billing claims. Automation is faster and more accurate.
What Timelines Apply For Submitting Clean Claims To Payers?
There is a timely filing limit for every payer. In the case of Medicare, it is usually one calendar year following the date of service. Yet, most individual payers, such as UnitedHealthcare or Aetna, can have restrictions as short as 90 or 180 days. You don’t have to wait until the resumption of an unclean claim. When you finally get it done, you may even be beyond the filing limit, which is to say that you will not receive a paycheck.
What Metrics Track Your Practice’s Clean Claim Rate?
To know if you’re successful, you must track your Clean Claim Rate (CCR).
The formula is: (Number of Claims Accepted on First Pass / Total Number of Claims Submitted) x 100. A healthy practice should aim for a CCR of 97% or higher. If you are below 90%, your RCM process needs an immediate overhaul.
What Documentation Prevents Common Clean Claim Rejections?
To ensure what is considered a clean claim stays clean, you need robust documentation. This includes:
- Current Referral/Prior Authorization numbers clearly listed in Box 23.
- Clear “Linkage” between the diagnosis and the procedure.
- Proof of medical necessity for “unlisted” codes.
What Are The Main Reasons Claims Become Unclean?
As is the case with me, there is a line often dictated by semantics between a dirty claim and an unclean claim, but the net effect of such is the same: no money.
- The Dirty Claim: This is generally a claim having egregious flaws, e.g., a signature omission or an invalid CPT code.
- The “Unclean Claim”: This may be technically correct in its structure, but it lacks the information that the payer needs to receive on a particular patient, like a primary EOB (Explanation of Benefits) or a secondary payer.
Conclusion
Understanding “what is a clean claim” is the foundation of a successful medical practice. Thus, you should not ignore its significance for a healthy RCM. Capline can help you increase the clean claim rate, so contact us now.
People Also Ask
1. What are the different types of claims in medical billing?
The two primary types are professional claims (837P/CMS-1500), used by individual physicians and practices, and institutional claims (837I/UB-04), used by hospitals and facilities. Both must meet “clean claim” standards to be paid.
2. What is the difference between clean and unclean claims?
A clean claim is error-free and processed without human intervention, leading to fast payment. An unclean (or dirty) claim contains errors, missing data, or discrepancies that lead to a rejection or denial by the payer.
3. What software tools help generate clean claims automatically?
Most modern Electronic Health Record (EHR) and Practice Management (PM) systems include built-in “scrubbers.” There are also standalone clearinghouse tools that perform deep claim scrubbing in medical billing to catch errors before submission



