Medical Billing Process in Healthcare Explained With 10 Simple Steps
If you run a dental clinic or a growing dental treatment brand, you already know this pain. Your chairs are full, your team is working hard, but your money still feels “stuck.”
Claims get denied, payments arrive late, patients get confused about what they owe, and your front desk spends hours fixing the same issues again and again.
That is exactly why the medical billing process matters so much. It is the system that turns care into clean claims and turns clean claims into real payments. And right now, denials are not rare. One 2025 claims survey shared by Experian found that 41% of respondents said at least 1 in 10 claims is denied, which means more rework, more follow-up, and more delayed cash flow.
What is Medical Billing?
Medical billing is the work of collecting, checking, and sending the right information so a provider gets paid for patient care. It connects the patient, the provider, and the insurance payer in one cycle. The goal is simple: make sure the hospital or doctor gets paid for services like diagnosis, treatment, lab tests, and outpatient care.
It also includes tasks like insurance checks, medical coding process, charge entry, claim submission, payment posting, and follow up. To say it in simple words, medical billing is “how the money moves” after the care is delivered.
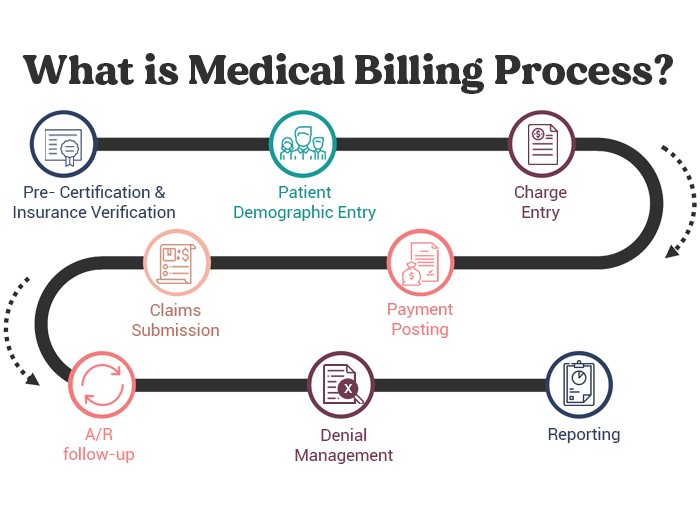
What is the Medical Billing Process?
The medical billing process is the full chain of steps that starts when a patient books or arrives, and ends when the balance becomes zero.
Types of Medical Billing in Healthcare
Even though the steps feel similar, billing can look different depending on the service.
- Professional billing (physician billing)
- Institutional billing.
- Dental billing
- Special cases billing
What Are the Steps in the Medical Billing Process?
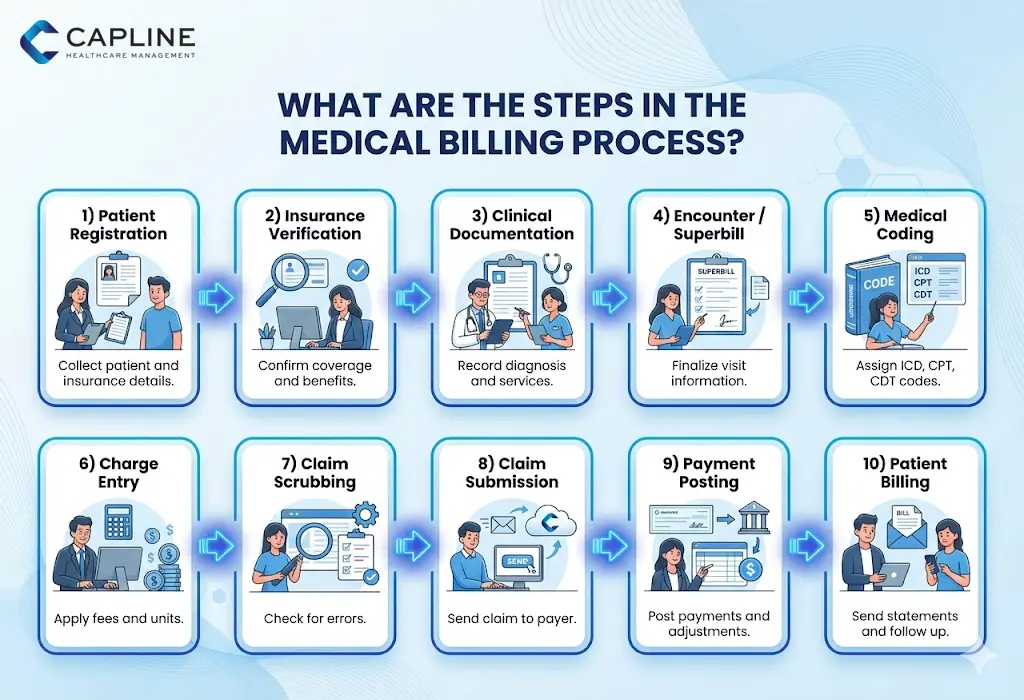
Below are the 10 steps in a clear, easy order. This structure matches common billing workflows and also aligns with business.com’s 10 step guide.
Step 1: Register the patient
This is where the whole medical billing process begins.
What you collect:
- Patient name, DOB, address, phone
- Insurance details
- ID numbers and plan information
For dental treatment brands, even a small typo in a member ID can lead to a denial later. Registration is not “just paperwork.” It is the first billing filter.
Step 2: Verify insurance and eligibility
Eligibility verification confirms:
- If the plan is active
- What the plan covers
- Copay, deductible, and benefits
- Whether pre authorization is needed
Capline lists eligibility and verification as a key part of the medical billing process. This step prevents surprise patient balances and cuts denials caused by inactive coverage.
Step 3: Record clean and complete documentation
Your clinical notes become the base of the claim. This includes:
- Diagnosis details
- Procedures done
- Materials used (important in dental)
- Provider signatures if needed
Missing details can cause claim rejections later, especially for services that need proof of medical necessity.
Step 4: Send encounter notes or superbill to billing
After the visit, your front office or EMR creates a superbill or encounter summary. This is where the physician billing process often breaks:
- Provider forgets to finalize notes
- Procedures are not captured
- Codes are missing or incomplete
Fast, clean handoff keeps billing on time.
Step 5: Do the medical coding process
This step converts the medical record into codes. That includes:
- Diagnosis codes (ICD)
- Procedure codes (CPT, CDT for dental)
- Modifiers when needed
This is where the medical coding process protects your claim. Coding must match documentation, payer rules, and the correct level of service.Even one wrong modifier can change payment or cause denial.
Step 6: Charge entry and charge capture
Now the claim gets its “price.” This includes:
- Procedure fee amounts
- Units
- Provider NPI and location
- Payer details
Step 7: Claim scrubbing and claim quality check
Before submission, the claim should be scrubbed. A good scrub checks:
- Missing patient info
- Wrong policy number
- Invalid codes
- Incorrect modifiers
- Duplicate claims
This step is a big reason why clean claims get paid faster.
Step 8: Claim submission to the payer
Now you send the claim to insurance. In the US medical billing process, most claims are filed electronically through clearinghouses. That speeds up processing and gives you tracking. Once submitted, the payer reviews it in a process called adjudication. Business.com lists payer adjudication monitoring as a key billing step.
Step 9: Payer adjudication and payment posting
Adjudication results in:
- Paid
- Denied
- Rejected
- Pending for more info
If paid, you get an ERA (electronic remittance advice) or an EOB (explanation of benefits). Then payment posting happens:
- Insurance payment is applied
- Adjustments are recorded
- The remaining patient balance is calculated
This is a major part of medical bill processing because it decides what the patient owes next.
Step 10: Patient statements and collections follow up
Once insurance finishes its part, patients may still owe:
- Copay
- Deductible
- Coinsurance
- Non-covered services
Business.com includes patient statements and payment follow up in the last steps of the cycle. For dental practices, clear patient billing matters a lot. Patients pay faster when:
- Statements are simple
- Charges are explained
- Payment options are easy
The Importance of the Medical Billing Process
A strong medical billing process is not only about money. It protects the clinic’s daily operations.
Here is why it matters:
- It protects cash flow: When claims are slow, your payroll and lab bills still come on time. Faster billing keeps the practice stable.
- It reduces denials and rework: Denials create extra admin work. Some claims report highlights that many denials come from missing or inaccurate data and authorization issues.
- It improves the patient experience: When eligibility is checked early, patients know what to expect. That reduces confusion and payment fights at the front desk.
- It keeps your practice safer: Accurate medical billing supports compliance and reduces the risk of audits and refunds.
Conclusion
The medical billing process is not just a back-office task. It is the system that keeps care sustainable. For dental treatment brands, it matters even more because one missed code or one wrong insurance detail can delay payment and increase patient complaints. If you focus on the 10 steps, maintain clean documentation, strengthen your medical coding process, and track the right metrics, your medical bill processing becomes faster and simpler.
You stop chasing money and start running a calmer practice. Want fewer denials and faster payments without the daily billing stress? Capline Healthcare Management can help you establish a cleaner, simpler billing cycle that ensures timely payment. Connect with us today.
People Also Ask
1. How long does the medical billing process take?
It depends on the payer and the claim type. Clean electronic claims can be processed in a few weeks, but claims with denials, missing info, or authorization issues can take much longer.
2. What are common medical billing procedures?
Common procedures in billing work include:
- Patient registration and eligibility verification
- Coding and charge entry
- Claim submission
- Payment posting
- Denial management
- Patient billing and follow up
These are the everyday building blocks of the US medical billing process.
3. What Role Does Medical Coding Play in the Billing Process?
The medical coding process turns treatment into a format insurance understands. If coding is wrong, the payer may deny or underpay the claim. Coding is the bridge between clinical work and billing payment.
4. What is the difference between medical billing and medical coding?
- Medical coding is choosing the right diagnosis and procedure codes from the medical record.
- Medical billing is using those codes to create the claim, submit it, track it, post payments, and bill the patient.
Both work together inside the medical billing process